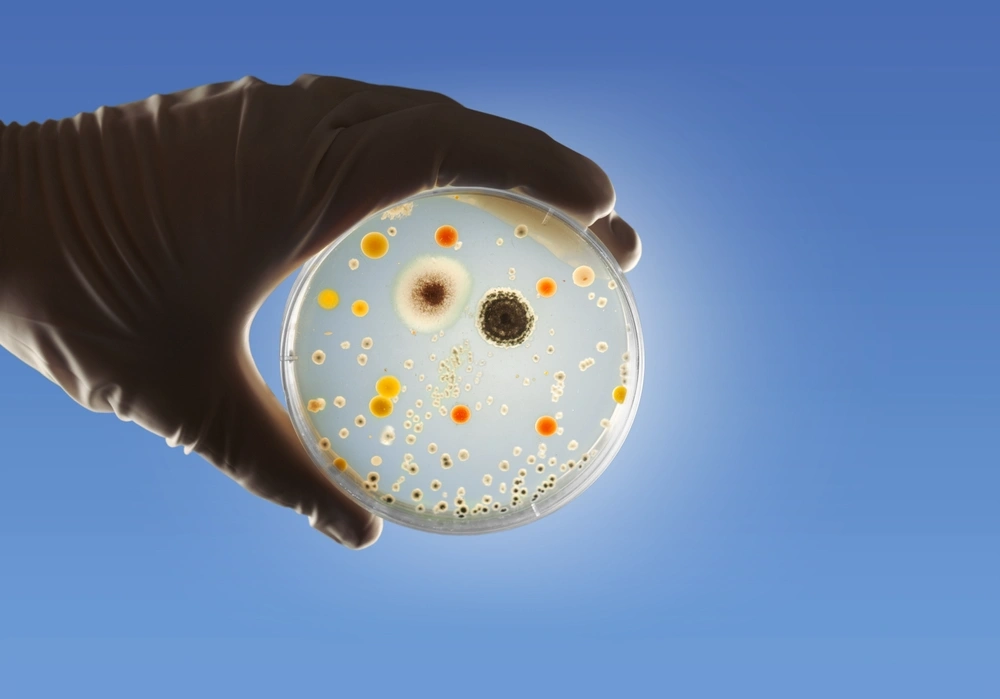
Flesh-eating bacteria can lead to necrotizing fasciitis, which might sound like something out of a horror movie, but it’s a real and serious medical condition that requires immediate attention.
Here’s what you need to know about this condition.
What is flesh-eating disease?
Flesh-eating disease, scientifically known as necrotizing fasciitis, is a rare but extremely dangerous infection.
Despite the flair in its name, it describes a serious bacterial infection that rapidly destroys the body’s soft tissues, such as the:
- Skin
- Fat
- Tissue surrounding muscles
The bacteria responsible for this condition, including Streptococcus pyogenes and other harmful types, typically enter the body through a break in the skin, like a:
- Cut
- Scrape
- Surgical wound
Once inside, these bacteria release powerful toxins that damage and kill cells, cut off blood flow, and cause the tissue to die. The infection spreads quickly, which is why early recognition and treatment for this condition is a matter of life and death.
What are the types of flesh-eating bacteria infection?
This infection can be classified into several types based on the bacteria that cause it. Here’s a breakdown of each type:
- Type I: Polymicrobial infection (multiple bacteria involved). Type I necrotizing fasciitis is the most common form and involves a combination of different bacteria working together to cause infection. It’s often seen in adults with chronic health conditions, like diabetes or immune system disorders, and progresses more gradually. While still very dangerous, this type typically requires a slightly different treatment approach due to the range of bacteria involved.
- Type II: Monomicrobial infection (Streptococcus pyogenes). Type II is caused primarily by Streptococcus pyogenes, also known as “Group A strep.” This type can develop rapidly and is more likely to affect healthy individuals with no underlying health conditions. Because it spreads so quickly, Type II necrotizing fasciitis requires immediate medical attention to prevent life-threatening complications.
- Type III: Caused by Vibrio vulnificus Type III necrotizing fasciitis is less common but very serious. It’s caused by Vibrio vulnificus, a bacteria found in warm saltwater environments. Infection can occur after exposure to contaminated water, especially if there’s an open wound. This type can progress very quickly and requires specific treatment to address the unique bacteria involved.
How do you get infected by flesh-eating bacteria?
Flesh-eating bacteria can enter the body in several ways, including the following:
- Through cuts or abrasions in the skin. Even a minor cut, scrape, or insect bite can serve as an entry point for these bacteria. If bacteria come into contact with a wound, they can invade the body’s soft tissues and lead to infection.
- By swimming in or exposure to contaminated water. Natural bodies of water, such as oceans, rivers, and lakes, as well as man-made pools, can sometimes contain flesh-eating bacteria. Open wounds provide easy access for these bacteria, so if you have a cut or open sore, avoid swimming or wading in potentially contaminated waters to lower the risk.
- During surgical or medical procedures in hospitals. Although rare, flesh-eating bacteria can enter the body during medical procedures if they come into contact with a surgical wound. Medical facilities follow strict sterilization practices, but post-surgical wound care is also critical to prevent infection.
What are the symptoms of a flesh-eating bacteria infection?
Symptoms of a flesh-eating bacteria infection appear quickly and can worsen in a short amount of time. Here’s what to look for:
- Intense pain out of proportion to the injury’s appearance. The pain caused by a flesh-eating bacteria infection is often much more severe than the visible wound or injury would suggest. This extreme pain can start suddenly and intensify rapidly, which signals that the infection is advancing below the skin.
- High fever and chills. Experiencing these is common as your body mounts an immune response to the severe infection.
- Rapidly spreading redness from the infection site. Within a few hours, the area around the wound may quickly become red, swollen and warm to the touch.
- Dark, blistered, or necrotic (dead) skin. As the infection progresses, the skin around the area may blister, darken, or develop patches of dead tissue, called necrosis. This is a serious sign that the bacteria are destroying healthy tissue, which can lead to even more severe complications if not treated.
Why is it dangerous?
Flesh-eating bacteria infections are extremely dangerous because of how quickly they spread and the severe damage they inflict on the body. If untreated, it could progress and lead to the following:
- Sepsis within hours
- Long-term disability
- Death
How is a flesh-eating bacteria infection diagnosed?
Here are different ways to diagnose flesh-eating bacteria infection:
- Tissue biopsy to identify the bacteria. With this procedure, your healthcare provider takes a small sample from the affected area to pinpoint the specific bacteria causing the infection, which is essential for choosing the right treatment.
- Blood tests to check for signs of infection. Your healthcare provider may order a blood test to detect signs of infection and inflammation in the body. Elevated levels of certain markers in the blood can indicate the body’s response to a serious infection.
- Imaging tests (MRI or CT scans) to view tissue damage. These tests help doctors see how much damage the infection has caused to muscles and tissues so they can decide on the next steps for treatment.
How is a flesh-eating bacteria infection treated?
Treating a flesh-eating bacteria infection requires aggressive and multi-step approaches to stop the fast-moving bacteria. Here’s an overview of the primary treatments:
- Broad-spectrum antibiotics. To fight off the infection, powerful antibiotics are given intravenously, which allows the medication to reach the bloodstream quickly. These antibiotics are broad-spectrum, meaning they target a wide range of bacteria, which is essential for an infection that progresses so rapidly.
- Surgical debridement. In many cases, doctors must perform a surgical procedure called debridement, which involves removing dead and infected tissue to contain the bacteria and stop it from spreading further through the body.
- Hyperbaric oxygen therapy. By breathing in 100% oxygen in a special chamber, the oxygen levels in your blood increase to create an environment that slows bacterial growth and supports tissue healing.
- When the infection is severe and tissue damage is extensive, amputation of the affected limb may be necessary. Although drastic, this step can be lifesaving as it prevents the infection from spreading further.
How can you prevent contracting a flesh-eating bacteria infection?
Here are simple ways to minimize the risk of bacterial entry and spread of the infection:
- Immediate washing and disinfecting of all wounds
- Avoiding natural bodies of water when you have an open wound
- Using protective barriers in high-risk environments
- Seeking timely medical intervention for suspicious wounds
Frequently asked questions
What causes infections by flesh-eating bacteria?
Infections by flesh-eating bacteria are caused by several types of bacteria, including Streptococcus pyogenes. These bacteria enter the body through breaks in the skin, such as cuts or scratches.
How quickly do symptoms of flesh-eating bacteria infection appear?
Symptoms of flesh-eating bacteria infections can appear within hours of infection. Early signs include severe pain and swelling, and the skin may become red, warm, and tender to the touch.
What are the treatment options for flesh-eating bacteria infections?
Treatment options for infections include powerful antibiotics administered intravenously and, in severe cases, surgical removal of dead tissue. Hyperbaric oxygen therapy may also be used to halt the bacteria’s progression.
Can flesh-eating bacteria infections be prevented?
Prevention of infections involves proper wound care, including cleaning all cuts and scrapes with soap and water, applying an antibiotic ointment, and covering wounds with a clean bandage until healed.
What is the mortality rate for flesh-eating bacteria infections?
The mortality rate for infections can be high, which can range from 20% to 30%. Factors influencing mortality include the speed of diagnosis, the patient’s overall health, and the promptness of treatment initiation.
Key takeaway
While flesh-eating bacteria infections are rare, they are extremely serious and demand immediate medical attention. Recognizing symptoms early, such as intense pain, rapid swelling, and skin discoloration, can make a lifesaving difference.
If you contract this infection, your treatment options include antibiotics, surgery, and, in severe cases, amputation to halt the infection’s spread.